
Wake Forest Institute Working on Regenerative Medicine Therapies for 40 Organs, Tissues
Human organ transplants became possible in 1954 when a kidney became the first organ to be transplanted successfully, eventually earning Boston physician Joseph Murray the Nobel Prize.
Today, it’s also possible to receive a transplanted heart, lungs, liver, pancreas or intestines, as well as tissues including skin, bone, corneas, tendons, ligaments and blood vessels.
A record-high number of organ transplants – 41,354 – were performed in the United States in 2021, according to the United Network for Organ Sharing, a nonprofit organization that supports the nation’s transplant system. It was the first year that organ transplants exceeded 40,000.

Despite the progress made in organ transplantation over the last seven decades, the demand for organs still greatly out-strips the supply, a trend unlikely to reverse.
“Even though organ transplants are out there, the challenge is that more patients are dying every day from organ failure, and the numbers are fairly shocking actually,” said Anthony Atala, M.D., an internationally acclaimed urologist, researcher and professor at the Wake Forest University School of Medicine. “So that’s where regenerative medicine comes in.”
Atala is director of the Wake Forest Institute for Regenerative Medicine (WFIRM), a translational research organization devoted to bringing new treatments and cures to patients with diseased or damaged organs or tissues. He highlighted WFIRM’s activities and impact as the keynote speaker at Triad BioNight, a dinner and awards event held June 23 at High Point University and sponsored by the North Carolina Biotechnology Center.
Atala's appearance at the event reinforced the mutual admiration between him and NCBiotech that dates back to his arrival at the Triad university in 2004. The Biotech Center has awarded numerous grants to various members of his lab over the years, and Atala has also served on the NCBiotech board of directors.
NCBiotech has provided $352,476.32 in grants to Wake Forest University for regenerative medicine-associated research during Atala’s 18 years at the university. The Center has awarded an additional $75,883.62 in meeting, event, and educational grants for regenerative medicine-related programming during the same time, including an active $10,000 award for an upcoming meeting.
“It is clear to see how over time, this regional effort has global impact,” said Nancy Johnston, executive director of NCBiotech’s Piedmont Triad Office. "New initiatives underway indicate there is power in partnerships and place; value in investing in innovation; and the top talent it takes in this emerging field of regenerative medicine."
Bringing technologies from bench to bedside
Atala told the crowd of nearly 400 attendees that WFIRM’s scientists, technicians and physicians are working on regenerative medicine therapies for about 40 different organs and tissues, building on 15 applications that have been used in patients to date.

“We have an amazing team – over 450 people – all working together to bring these technologies from the bench to the bedside,” Atala said.
WFIRM is based in a five-story building spanning about 200,000 square feet in Winston-Salem’s Innovation Quarter, a downtown district devoted to research and technology enterprises.
“We do everything here, from the idea, to the concepts, to the proof of principle at the benchtop, to the preclinical work, all the way to the manufacturing of the product in an FDA-compliant facility right in this building,” Atala said.
WFIRM scientists and physicians made history in 1999 when they were the first in the world to implant laboratory-grown organs into humans. Seven children with spina bifida and severely malfunctioning bladders received grafts of rudimentary bladders engineered in Winston-Salem.
Today WFIRM’s multidisciplinary work uses cells, bioreactors, tissue engineering, biomaterials, 3D bioprinting, small molecules, gene editing, body-on-a-chip technologies and personalized medicine approaches to innovate new therapies and diagnostics.
Cell therapy innovations
Cell therapy – the use of harvested and cultured cells to restore tissues and organs – is a major thrust of WFIRM’s work. The technology offers a great advantage over donated organs and tissues because it typically uses a patient’s own cells, thereby avoiding rejection by the body’s immune system.
Work is under way at WFIRM to use skeletal muscle cells to restore lost muscle function in patients with urinary incontinence and in patients undergoing rotator cuff repair surgery.
In both cases, skeletal muscle cells are collected from a tissue sample smaller than a postage stamp, are multiplied in the lab, and are then injected into the body to build muscle.
Researchers are also working with a type of stem cell taken from the amniotic fluid or placenta after a woman gives birth. WFIRM scientists were the first in the world to identify and characterize stem cells derived from amniotic fluid in 2007 and since then have developed techniques for isolating and expanding the cells.
“These cells are very powerful,” Atala said. “They can grow into all three different major categories of cells that lead to every cell in your body.”
WFIRM is investigating the use of these cells as potential therapies for patients with chronic kidney disease.
Cell therapy often involves the use of biomaterials that can be shaped into scaffolds that mimic the shape of a tissue or organ. Different materials can be mixed and matched for various tissue reconstruction.
One application is for helping patients with a damaged urethra, the duct that drains urine from the bladder. A tubular-shaped scaffold is coated inside and outside with muscle cells that are taken from the patient and multiplied, then the scaffold is placed in an oven-like device to encourage cell growth.
“It’s very much like baking a layer cake,” Atala said, eliciting chuckles from the audience. “Once it’s completed you actually put it back into the patient.”
The implanted scaffold biodegrades in the body after six months, but the cells remain viable indefinitely. “You end up with your very own cells, your very own bridge and your very own organ,” Atala said.
WFIRM researchers have successfully engineered replacement tissues and organs of all four shapes found in the body – flat structures, tubular tissues, hollow organs and solid organs.
3D bioprinting and organs on chips
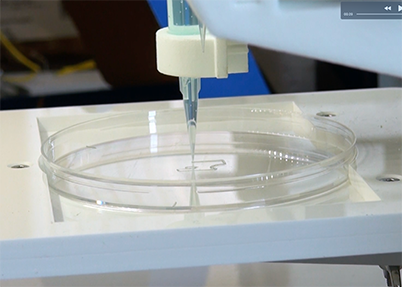
WFIRM is also a pioneer in 3D bioprinting, the use of printer-like devices to deposit layers of living cells in three-dimensional patterns. The invention, inspired by desktop ink jet printers, brings precision and automation to the construction of tissues and organs.
Last year two teams of scientists from WFIRM used 3D bioprinting to win first and second place in NASA's Vascular Tissue Challenge, a national competition to accelerate tissue engineering innovations that might benefit people on Earth today and space explorers in the future.
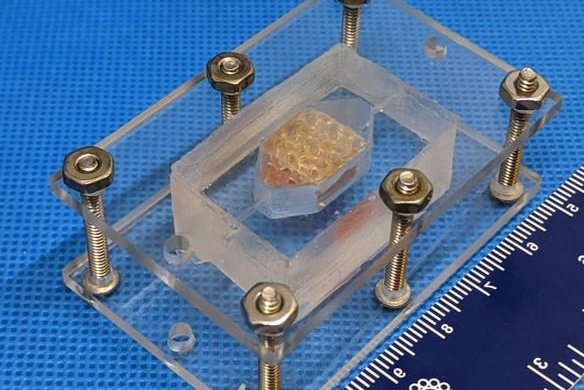
The WFIRM teams created lab-grown human liver tissues that were strong enough to survive and function in ways similar to those inside the body. They each used a varied 3D printing technique to construct a cube-shaped tissue about one centimeter thick and capable of functioning for 30 days in the lab.
“That was a major challenge,” Atala said, because “anything over the size of a pinhead will not get nutrition.”
Tissues in the body rely on blood vessels to supply cells with nutrients and oxygen and remove metabolic waste. Recreating this process in engineered tissue is difficult, so NASA asked teams to develop and test strategies for making tissues with functional artificial blood vessels.
The winning teams used 3D printing to create gel-like molds with a network of channels designed to maintain sufficient oxygen and nutrient levels to keep the constructed tissues alive.
The two teams collectively won $400,000 while no other team in the national competition qualified for third place.
Another WFIRM application of 3D bioprinting is body-on-a-chip technology, which applies cells onto a computer chip to mimic organs.
“We can create miniature hearts, lungs, blood vessels, kidneys and brains, put them all together on a chip and actually start to screen drugs over time,” Atala said.
The technology can also be used to create tumors on a chip for personalized medicine. Tumor cells harvested from tissue biopsied at the time of a patient’s cancer diagnosis are applied to a chip and then tested against various chemotherapy drugs “so we can best predict what the best treatment is for that patient, before that patient gets the treatment,” Atala said.
The cell therapy, 3D bioprinting and body-on-a-chip technologies are “just a sampling” of WFIRM’s work, and “we have a lot of things going on,” Atala said.
“Our mission is to bring these technologies to patients, to improve patients’ lives through regen med,” he said. “Our vision is to lead a global transformation from treatments to cures.”
A major resource
Beyond its own research, WFIRM has become a major influencer and resource in regenerative medicine nationally and globally.
It has over 400 research collaborations with scientists across the United States and around the world.

“For most of these collaborations, WFIRM is the one that’s providing materials, reagents, cells and know-how, trying to disseminate this information to a global scale, Atala said.
WFIRM also helps prepare the next generation of regenerative medicine scientists through education and training programs for high school students, undergraduates, graduate students and post-doctoral fellows. It also sponsors conferences and workshops, provides content and materials for museum exhibits around the world and publishes textbooks.
The institute has spurred new initiatives and entities in Winston-Salem to advance regenerative medicine nationally and globally. This ecosystem, called the Regenerative Medicine Hub, includes the nonprofit RegenMed Development Organization (ReMDO), a research partner with WFIRM that sponsors several programs to advance the field nationwide, including the Regenerative Manufacturing Innovation Consortium and the Regenerative Medicine Manufacturing Society.
Through its RegeneratOR initiative, ReMDO sponsors three programs to support startup and growth companies in regenerative medicine:
- The RegeneratOR Test Bed provides companies access to advanced biomanufacturing equipment, talent, and programs to support prototyping and initial product development.
- The RegeneratOR Innovation Accelerator encourages innovation by providing space and support, including market potential validation, benefit analysis, financial planning, budgeting and business plans.
- The RegeneratOR Workforce Development program provides skilled talent through training programs and by connecting colleges, university programs and technical schools with biomanufacturing staff, engineers and research leaders.
These and other resources in the Regenerative Medicine Hub have attracted about 30 bioscience companies to Winston-Salem’s Innovation Quarter, ranging from local start-ups to multinational corporations.
The latest company to establish a presence at ReMDO’s Innovation Accelerator is Houston-based Axiom Space, developer of the first commercial space station that will supplement and eventually replace the International Space Station.
Axiom will partner with WFIRM and ReMDO to focus on innovations in regenerative medicine manufacturing in space. Research done on the new space station, in low orbit 250 miles above Earth, will be free from the constraints of gravity, providing potential benefits.
A growing industry
WFIRM and Winston-Salem have staked an early claim in a promising industry that appears destined for robust growth.
Various consultants’ reports predict the global market for regenerative medicine will expand at a compound annual growth rate ranging from 9 to 23% during this decade. By 2030 the market will be worth up to $150 billion, according to a report by Verified Market Research of Jersey City, N.J.
Driving that growth are an aging population battling chronic diseases, rising investments in regenerative medicine research, and advances in new technologies and therapies such as those being developed by WFIRM.
“Regenerative medicine is an emerging field,” Atala said. “We’re still trying to figure out what is the best next thing that we can do to advance these technologies.”
