
WFIRM Team Wins Huge NASA Vascular Tissue Challenge
Five years ago, the National Aeronautics and Space Administration put up prize money and created a contest to see if regenerative medicine researchers could turn human cells into blood vessels – and someday, maybe, human organs for space travelers.
Over those five years, 11 teams have entered NASA’s Vascular Tissue Challenge, developing and refining their techniques to meet this previously unmet goal.
Now, however, Team Winston of the Wake Forest Institute for Regenerative Medicine (WFIRM) has succeeded, winning the $300,000 first-place prize. And Team WFIRM, also from WFIRM, won the second place $100,000. Both teams were led by Anthony Atala, M.D., director of WFIRM and a member of the North Carolina Biotechnology Center board of directors. No other team completed the challenge.
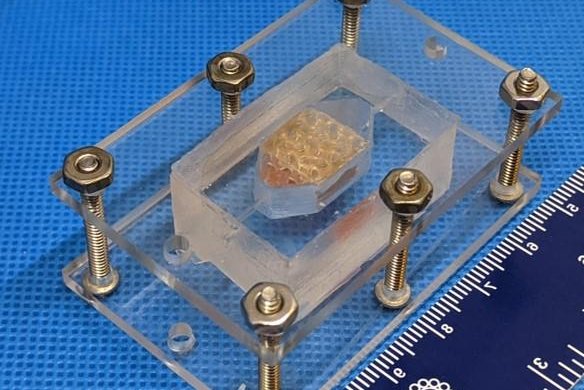
Team Winston used this chamber to hold the printed tissue and test its perfusion.
– WFIRM photos
“The vascular tissue challenge is about incentivizing the public to develop thick, functional tissue that can one day, perhaps, help us achieve long-duration missions, keep our astronauts healthy and have amazing earth applications,” explained Monsi Roman, NASA’s Centennial Challenges program manager, in NASA’s Science Live streaming.
NASA established multiple criteria for the Vascular Tissue Challenge. The 1-centimeter sample of human tissue, about the width of an average adult woman’s pinkie finger, must be functional for at least 30 days in-vitro, or outside of a living organism. Also, it has to be vascularized, or contain tissue with its own blood vessels, which requires more than one type of cell.

“The research progression we made in a short period of time was possible because the NASA challenge provided an opportunity to push our teams forward to think differently and come up with creative approaches,” said Atala. “With two different 3D printing methods, our teams succeeded in creating complex, perfused tissue, an important step forward for future tissue engineering research and patient care.”
Engineering human tissues can allow researchers to study virtually any disease. The samples created by Teams Winston and WFIRM function in-vitro just as they do in the body, which allows therapies to be tested on vascular tissue samples rather than on patients. As a result, better therapies can be produced for people living with a disease.
Vascular tissues allow other tissues to grow, so this seemingly miniscule sample is the starting point to growing entire organs outside the body. Applications include pharmaceutical testing, disease modeling and organ transplant technology.
According to Dave Gobel, founder and chief executive officer of the Methuselah Foundation which teamed up with NASA, scientists will be able to make tissue patches for the liver in the next five to 10 years. These tissue patches could be added to sick organs, for the organ to either recover itself or provide more time for a transplant to become available.
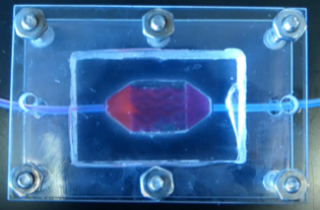
fluid passing through the tissue without leaking.
In 10 to 15 years, Gobel says, whole livers and kidneys could be manufactured, offering an alternative to the hundreds of thousands of people who are in need of a transplant. Organs grown from a patient’s own cells would eliminate the need for a lifetime of immunosuppressant drugs, which keep the body from rejecting the foreign organ but also weaken the immune system.
NASA has a unique interest in this technology because of how space conditions, including radiation and zero gravity, impact human cells. In the short term, this technology can help astronauts working at the International Space Station, whose organs are not functioning at their full potential. Researchers will also be able to study the impact of space conditions on humans without having to send anyone into space. Instead, researchers would send the tissue sample. In the long term, vascular tissue technology can help maintain the health of an astronaut crew when they explore Mars and beyond.
The winning approach
All teams took vastly different approaches in creating their technologies, including holographic laser projections, bioreactors and a combination of genetic engineering and 3D printing. Team Winston used bioprinting to create their sample.

Kelsey Willson, Ph.D., a WFIRM grad student on Team Winston, broke down her winning team’s process during NASA’s Science Live.
“In this tissue, we used two kinds of cells,” she says. “Endothelial cells make up blood vessels and hepatocytes are the primary cells found in the liver.” Different cells prefer different conditions, so the team had to create an environment that would satisfy both.
Early on, Team Winston, led by James Yoo, M.D., Ph.D., had to decide what shape would be best for getting fluid flow and nutrients in and out of the sample, while meeting the 1-centimer cubic requirement.
“We settled on a gyroid shape, which is a series of interconnecting wave-like tubes,” Willson says. “Then, we looked at the best gel for allowing our cells to grow, expand and communicate with each other, which ended up being a modified gelatin.”

Then, Team Winston built a circulation system similar to that of the human body. They nurtured the sample until it met all of NASA’s size and functionality requirements.
“This was one important step of many on the path inward to improve medicine in the body and upward into space,” Maria Price Rapoza, Ph.D., told the North Carolina Biotechnology Center. Rapoza served as a member of the judging committee. She is the executive director of the Duke Cardiovascular Research Center and former vice president of Science and Technology Development at NCBiotech. “It was incredibly rewarding to see all the teams compete in this difficult challenge.”
The next step in developing this vascular tissue is appropriately integrating the in-vitro cells into the body.

For coming in first place, Team Winston’s sample will be sent to the ISS to test the effects of microgravity on vascular tissue. In the meantime, team members are integrating this technology into other projects. Willson is working on 3D-printing skin with hair follicles in it. Young-Wook Moon, Ph.D., Team Winston member and WFIRM research fellow, is applying this gyroid shape to neural tissue to develop a blood-brain barrier prototype, which would allow the passage of essential nutrients to the brain while protecting it against toxins.
“I cannot overstate what an impressive accomplishment this is,” says Jim Reuter, NASA associate administrator for space technology, in an article. “When NASA started this challenge in 2016, we weren’t sure there would be a winner. It will be exceptional to hear about the first artificial organ transplant one day and think this novel NASA challenge might have played a small role in making it happen.”
