
Feds Award $24M for Wake Forest Lung-On-A-Chip Studies
of toxins on human lungs and to develop treatments. -- WFIRM photo
The Wake Forest Institute for Regenerative Medicine (WFIRM) in Winston-Salem has won $24 million in federal funding to model the effects of chlorine gas on human lungs and to develop treatments for chemical injury.
Chlorine gas has been used in warfare, is a potential weapon for terrorists and is an ongoing threat to public safety due to accidental leaks of the widely used industrial chemical.
The five-year research program will be funded by the Biomedical Advanced Research and Development Authority (BARDA) within the Department of Health and Human Services’ Office of the Assistant Secretary for Preparedness and Response. The program will begin with a $13.5 million contract for the first two years, according to a news release from Wake Forest University.
Lung-on-a-chip technology
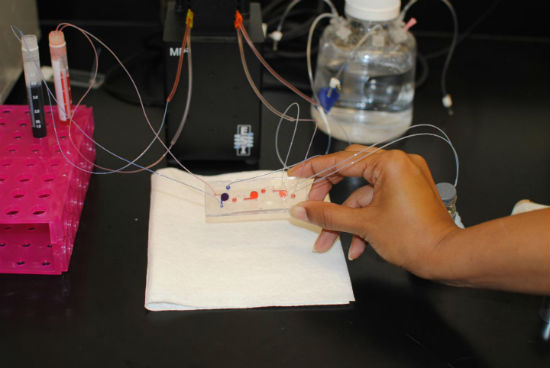
Researchers will use WFIRM’s lung-on-a-chip technology, which can model normal and diseased tissue, innate immune system response and reaction to drugs and toxins.
"Our lung-on-a-chip technology has grown out of our body-on-a-chip research, a system of miniature human organs created in the laboratory that can be used to further our understanding of the effects of inhaled chlorine gas and other toxins, as well as potential treatments," said Anthony Atala, M.D., director of WFIRM.
Currently, respiratory health, diseases and treatments are studied mainly in animal models or two-dimension (2D) cell culture models. The body-on-a-chip system overcomes the limitations of these models.
It uses human cells to create tiny 3D organ-like structures called tissue equivalents that mimic the function of the heart, liver, lung, blood vessels and other organs. Placed on a 2-inch chip, these structures are connected to a system of fluid channels and sensors that provide online monitoring of individual organs and the overall organ system.
A circulating blood substitute keeps the cells alive and can be used to introduce chemical or biological agents, as well as potential therapies, into the system. Hollow channels guide toxins or therapies under study from one tissue to the next, and sensors measure temperature, oxygen levels, pH and other factors in real time.
"We look forward to pursuing the long-term goal of this research with BARDA, which is to reduce the overall burden of in vivo testing (in living organisms) in the development and management of products for human clinical use and to speed up the development of treatments," Atala said.
A lethal chemical
Chlorine gas was used as a weapon during World War I and has been used repeatedly during the ongoing civil war in Syria. In addition, the large volume and ready availability of manufactured chlorine make the chemical a potential national security threat in the hands of terrorists.
Furthermore, chlorine is one of the most-used industrial gases in the United States and causes multiple deaths and injuries due to accidental leaks and household exposure. In 2005, a train collision in Graniteville, S.C., caused a tank car containing chlorine gas to leak about 60 tons of the chemical, killing nine people and injuring at least 250 more.
A leader in regenerative medicine
WFIRM is recognized internationally for translating scientific discoveries in regenerative medicine into clinical therapies. More than 450 scientists from around the world collaborate with the institute, working on more than 40 different tissues and organs.
A number of the basic principles of tissue engineering were developed at the institute, which has successfully engineered all four types of replacement tissues and organs - flat structures, tubular tissues, hollow organs and solid organs.
WFIRM was the first in the world to develop and implant an engineered organ into a patient. Patients have received nine different cell/tissue therapies developed at WFIRM, including skin, urethras, cartilage, bladders, muscle, and vaginal organs.
The institute’s body-on-a-chip research team received a Research and Development Excellence award in June at Triad BioNight, a celebration of the region’s life science industry organized by the Piedmont Triad Office of the North Carolina Biotechnology Center.
