
NC Team with NCBiotech Support Building a Better Bassinet

by a dedicated group of NC caregivers and inventors. -- Shutterstock
An innovative hospital bassinet promises to better support new families through enabling breastfeeding, skin-to-skin contact and mother-infant bonding, while improving newborn safety.
The Couplet Care Bassinet is designed to remove significant structural barriers for mothers and infants in hospital postnatal units. This includes making it easier, more comfortable and safer for mothers to access their infants and develop a strong breastfeeding relationship than experienced with use of existing hospital bassinets. The unmet need is especially pronounced for mothers experiencing pain and/or limited mobility from Cesarean section (C-section) or complicated vaginal deliveries. All new mothers are fatigued and deserve enabling environments.
A $100,000 grant from the North Carolina Biotechnology Center supported stakeholder feedback, design refinements, prototype manufacture, and pilot testing. According to Kristin Tully, Ph.D. and Catherine Sullivan MPH, RD, LDN, IBCLC, FAND, leaders of the project, bassinet testing will begin in 2021 under the direction of Amanda Thompson, Ph.D., at N.C. Women’s Hospital, in Chapel Hill, and Vidant Medical Center, in Greenville.
Development of the bassinet is a story of a methodical, evidence-based and human-centered design process involving a diverse inter-university collaboration and support from many sources.
“What we have been able to achieve is the result of thoughtful collaboration,” explained Ty Hagler, principal of Trig, a Triangle-based industrial design firm on the bassinet team.
Why a new bassinet design?
“The design currently in use in hospitals is a cart with a clear acrylic tub on top of it. It’s really meant for use by someone standing up and bending over it to care for the baby,” said Hagler.
The problem is that this design is not easy to use for a mother in the postnatal unit. She has only two options, both of which are uncomfortable, even painful, to access her baby. One is to get out of bed, stand and lean over to pick up the baby. Then, while trying to hold the newborn safely, reposition herself back into bed for breastfeeding or other infant care. This barrier has associated risks for dropping the baby and can make maternal recovery from childbirth more difficult, especially C-sections. The other way women are expected to use existing bassinets involves her twisting in bed and reaching out and over the high walls of the bassinet to lift the baby and bring it to her lap. New mothers should be able to see and touch their babies, enabling responsive parenting and recognition of hunger cues.

Tully’s research with colleagues in the United Kingdom has measured how the discomfort and stress of these access difficulties lead to less-frequent breastfeeding and other suboptimal health outcomes for both mother and baby. Tully also notes how the unnecessary obstacles posed by using current bassinets is a health equity issue.
“Many moms don’t have an attentive partner with them in the hospital, especially overnight, to contribute to care. Others may not feel empowered or otherwise able to request nursing assistance. If they’re not English-speaking, they also may not feel as comfortable hitting the ‘call’ button and saying what they need. So, sometimes they fall asleep with babies in their arms in the hospital because it hurts too much to move,” said Tully.
“We call it the Couplet Care Bassinet,” said Tully, “because couplet care is the term used in hospitals for the clinical approach of tending to the needs of moms and babies together.” She believes this new design will become the industry standard and facilitate immediate and sustained change in practice.
The bassinets in current use were designed decades ago for a hospital nursery setting before adoption of the standard of care practice of “rooming-in” in postnatal units. Rooming-in involves mothers and newborns spending 24 hours a day together in the absence of medical need for separation. It is one of the practices in the Baby-Friendly Hospital Initiative launched by the World Health Organization and UNICEF in the 1990s to motivate facilities worldwide to encourage and support breastfeeding. Having the baby in the same room provides easier access for mothers to more frequently nurse, learn and respond to infant cues and bond through skin-to-skin contact.
Extensive research supports breastfeeding and skin-to-skin contact between mothers and newborns as leading to healthier outcomes for both. Hospitals earn designation as Baby-Friendly by implementing the 10 practices, such as rooming-in, and skin-to-skin contact. The practices support mothers in initiation of breastfeeding and learning to manage common difficulties. According to Baby-Friendly USA, in 2020, 29% of babies will be born in over 600 designated facilities.
The American Academy of Pediatricians (AAP) recommends exclusive breastfeeding as the source of babies’ nourishment for the first six months and continued breastfeeding with the addition of complementary foods to 12 months and beyond.

The benefits of breastfeeding include decreased risk of lower respiratory infections, gastroenteritis, and otitis media (ear infections). Breastfeeding also reduces risks of sudden infant death syndrome, obesity, asthma, certain childhood cancers, diabetes, and post-neonatal death, according to a 2017 AAP report.
While breastfeeding is the biological norm for human mothers and babies, it does require some learning, practice, and support for optimal outcomes. Barriers to that process, especially initially after birth, can significantly affect whether mothers are able to successfully initiate and continue to realize their infant feeding goals.
Tully is a research associate at Carolina Global Breastfeeding Institute (CGBI) at the UNC Gillings School of Global Public Health. She led a study at Durham University in England during her doctoral work in which “side-car” bassinets attached to the side of the hospital bed improved the mother-newborn experience and reduced infant handling risks. Her research included observational work, studying mothers and babies with infrared cameras overnight in the hospital and at home to study patterns of behavior and breastfeeding.
Results of this research -- highlighted by the AAP – and because of an innovation gap in the U.S. market, led Tully to decide to create a new and improved bassinet for U.S. hospitals. She says, “We want to offer a real solution.”
Development of Prototype I
Using results from the research in England, Tully was supported by CBGI in establishing an interdisciplinary team across UNC-Chapel Hill, including Catherine Sullivan, director of CGBI; Carl Seashore, M.D., professor of pediatrics; and Alison Stuebe, M.D., MSc, associate professor of maternal-fetal medicine and medical director of lactation services at UNC Health Care. The team partnered with North Carolina State University industrial design graduate students. Sharon Joines, Ph.D., associate dean of the College of Design, led students in work using Tully’s research and federal regulations to develop a prototype. The North Carolina Translational and Clinical Sciences Institute funded this first phase of the project, beginning in 2016.
During the design process, the graduate students were briefed by the team about mother-infant needs and clinical processes, then they observed a maternity bed and infant bassinet in an empty patient room in the hospital. They also worked in the studio with a hospital bed and bassinet for ideation and prototype development. And, they invited new mothers, fathers and health care providers to the studio to ask them questions and to brainstorm. The project team then provided feedback on the initial student design ideas, which led to a second round of designs by the students.
At the end of the semester, the students presented 10 designs to the team and to business advisors, including Don Holzworth and Jan Davis, and designers from Trig.
Refinements Led to Prototype II
The next phase of the project involved testing of the first prototype.
Recent mothers were invited to come into the hospital and interact with the first prototype and a doll. The doll is one used for lactation training classes and has realistic features. Additionally, the team collected data from mothers and health care providers across the U.S. through an online survey and engaged with national maternity care leaders through webinars and in person.
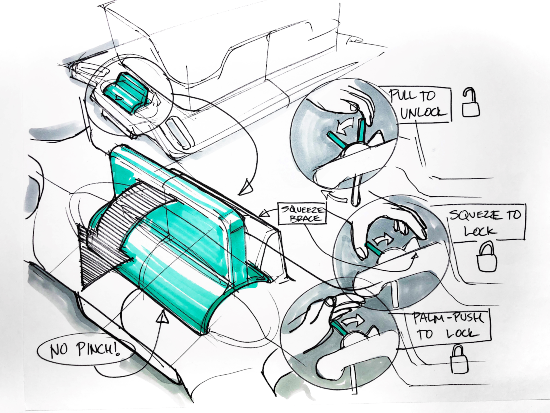
Hagler said data from this phase of the project led to major changes for development of Prototype II, including rethinking the control handles. Because his firm operates virtually, with each person working from their respective home offices, he said they used equipment at Hangar6 to build the second prototype.
Hangar6 is a Research Triangle-based prototyping and design assistance space created by the First Flight Venture Center science and technology incubator. It enables designing, building and modeling product prototypes using tools, such as a bio-compatible 3D printer, necessary for this project.

at Hangar6.
The team is now leveraging BIG support with a Phase I Small Business Innovation Research (SBIR) grant (R43HD097017). Hagler and Tully are co-principal investigators on the Phase 1 SBIR through the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health. The goal of a Phase I SBIR, according to NIH, is “to establish the technical merit, feasibility and commercial potential” of the project prior to awarding larger federal support for commercialization. The project includes engaging with health care providers and recent mothers in multiple North Carolina hospitals for design feedback, prototype refinement, and pilot use.
The patent process is underway in collaboration with the UNC Office of Technology Commercialization, Blackstone Entrepreneurs Don Holzworth and Jan Davis, and Trig.
“We think this will shift the landscape for maternity care,” said Tully. “The point is to better support women and their families. That is the bigger vision.”
Other funding for this project includes the Gillings Entrepreneurship Award through the UNC Gillings School of Global Public Health, CGBI, donor gifts, and the One N.C. Small Business Program.
